Rheumatoid arthritis (RA) affects 2.1 million Americans, three times more women than men. Onset is usually in middle-age, but often occurs in the 20s and 30s. RA is an inflammatory disease that causes pain, swelling, stiffness, and loss of function in the joints. It has several special features that make it different from other kinds of arthritis. For example, RA generally occurs in a symmetrical pattern which means that if one knee or hand is involved, the other one is also. The disease often affects the wrist joints and the finger joints closest to the hand but can also affect other parts of the body besides the joints. It can be accompanied by fatigue, occasional fever, and a general sense of not feeling well (malaise).
Inflammatory arthritis, which includes rheumatoid arthritis, are the most serious of the joint diseases. The disease is characterized by pain, swelling and morning stiffness lasting more than an hour. In addition, the symptoms are predominant in the morning and there is a tendency to fatigue through the day.
RA varies a lot from person to person. For some it lasts only a few months to a year or two and goes away without causing any noticeable damage. Others have mild or moderate disease, with periods of worsening symptoms, called flares, and periods in which they feel better, called remissions. Still others have severe disease that is active most of the time, lasts for many years, and leads to serious joint damage and disability.
Although RA can have serious effects on a person’s life and well-being, current treatment strategies – including pain relief and other medications, a balance between rest and exercise, and patient education and support programs – allow most people with the disease to lead active and productive lives. In recent years, research has led to a new understanding of RA and has increased the likelihood that, in time, researchers can find ways to greatly reduce the impact of this disease.
The Development and Progression of RA
Researchers suspect that some type of microorganism may be the trigger in some people who have an inherited tendency for the disease. Dr. Hoekstra, MD has found that virtually all the patients he has studied have had significant amounts of a bacteria called Propioni bacterium acnes. “This is the genus and species of the organism we believe is responsible for propagating and perpetuating this disease,” says Dr. Hoekstra. “It is a very common bacteria in an altered state of being – it is cell wall deficient.”
The bacterium was first identified and described in 1981 by G.A. Denys at Wayne State University in Detroit, Michigan. “This bacteria is passed transplacentally, from mother to fetus, and this may be responsible for RA showing up in generations in a single family,” says Dr. Hoekstra. Why this bacteria is prevalent in seemingly all cases of RA is not clear; but overuse of antibiotics may be a factor encouraging its growth. “The use of antibiotics is one of the most potent ways of inducing cell wall deficiency; bacteria seem to do this as a survival mechanism.” In other words, when a bacterium is transformed into a cell wall deficient form, it assumes different characteristics from the whole or native type of microorganism it used to be.
Dr. Hoekstra explains, “The organism remains intact except for losing its cell wall and its antigenic characteristics, enabling it to function as a cellular chameleon.” When it loses its antigenic signature, the bacteria are able to mask themselves against destruction by the immune system‘s antibodies which can no longer recognize them as antigens (foreign proteins).
Dr. Hoekstra’s mentor, Lida Holmes Mattman, Ph.D., also of Wayne State confirmed the causal role of P. acnes in a laboratory experiment. Dr. Mattman extracted the bacteria from the synovial fluid (which lubricates joints) of human arthritis patients, and injected it into chicken embryos. The chicks then exhibited symptoms of RA. When she treated the chicks with antibiotics known to disable P. acnes, the disease disappeared.
Another recently discovered aspect of RA is that sufferers who were previously thought to have overactive immune systems, instead may have exhausted immune systems. ”What this study has shown for the first time is that patients with RA have prematurely aged immune systems” said lead author Dr. Cornelia Weyand, a rheumatologist at the Mayo Clinic.
”Until now we have thought that these patients had overactive immune systems, which is why we have aggressively treated the symptoms of rheumatoid arthritis with medications that suppress the immune system.” Weyand and colleagues studied the immune systems of 51 patients with rheumatoid arthritis and compared them to 47 people of similar age who did not have the condition. They found that the T-cells – the immune cells that are programmed to recognize and attack invaders such as bacteria and viruses – were worn out. ”They do not make new T-cells.”
A normal joint (the place where two bones meet) is surrounded by a joint capsule that protects and supports it. Cartilage covers and cushions the ends of the two bones. The joint capsule is lined with a type of tissue called synovium, which produces synovial fluid. This clear fluid lubricates and nourishes the cartilage and bones inside the joint capsule.
In cases of RA, the immune system for reasons unknown attacks a person’s own cells inside the joint capsule. White blood cells that are part of the normal immune system travel to the synovium and cause a reaction. This reaction, or inflammation, called synovitis, results in the warmth, redness, swelling, and pain that are typical symptoms of RA. During the inflammation process, the cells of the synovium grow and divide abnormally, making the normally thin synovium thick and resulting in a joint that is swollen and puffy to the touch.
As RA progresses, these abnormal synovial cells begin to invade and destroy the cartilage and bone within the joint. The surrounding muscles, ligaments, and tendons that support and stabilize the joint become weak and unable to work normally. All of these effects lead to the pain and deformities often seen in RA. Doctors studying RA now believe that damage to bones begins during the first year or two that a person has the disease and this is one reason early diagnosis and treatment are so important.
Other parts of the body
Some people also experience the effects of RA in places other than the joints. About one-quarter develop rheumatoid nodules, bumps under the skin that often form close to the joints. Many people with RA develop anemia, or a decrease in the normal number of red blood cells. Other effects, which occur less often, include neck pain and dry eyes and mouth. Very rarely, people may have inflammation of the blood vessels, the lining of the lungs, or the sac enclosing the heart.
What are the signs and symptoms of RA?
- Pain and stiffness lasting for more than 30 minutes in the morning or after a long rest.
- Tender, warm, swollen joints. Joint inflammation often affecting the wrist and finger joints closest to the hand; other affected joints can include those of the neck, shoulders, elbows, hips, knees, ankles, and feet. Rheumatoid nodules are sometimes present.
- Symmetrical pattern. For example, if one knee is affected, the other one is also.
- Fatigue, occasional fever, a general sense of not feeling well (malaise).
- Symptoms possibly lasting for many years.
- Symptoms affecting other parts of the body besides the joints.
How is RA diagnosed?
RA can be difficult to diagnose in its early stages for several reasons. First, there is no single test for the disease. In addition, symptoms differ from person to person and can be more severe in some people than in others. Furthermore, symptoms can be similar to those of other types of arthritis and joint conditions, and it may take some time for other conditions to be ruled out as possible diagnoses. Finally, the full range of symptoms develops over time, and only a few symptoms may be present in the early stages.
Doctors use a variety of tools to diagnose the disease and to rule out other conditions: medical history, physical examination, laboratory tests. One common test is for rheumatoid factor, an antibody that is eventually present in the blood of most RA patients. Not all people with RA test positive for rheumatoid factor, especially early in the disease; indeed some who do test positive never develop the disease.
Other common tests include some that indicate the degree or severity of inflammation in the body (the erythrocyte sedimentation rate, or C-reactive protein), a white blood cell count, and a blood test for anemia. X-rays can be used to determine the degree of joint destruction but are not useful in the early stages of RA before bone damage is evident. They can be used later to monitor the progression of the disease.
Tea and decaffeinated coffee intake were individually associated with an increased risk of developing rheumatoid arthritis in a prospective study of 64,000 black women followed for up to 4 years. Caffeinated coffee intake was not associated with the risk of developing RA.
Signs, symptoms & indicators of Rheumatoid Arthritis

High ESR or elevated ESR

(Mildly/highly) elevated ANA levels or normal ANA levels

Weak appetite

Fatigue on light exertion

Recent swollen/painful lymph nodes

Itchy eyes

Discharges from eyes
Counter Indicators
Moist eyes
“Dry eye” is a symptom of certain autoimmune diseases like rheumatoid arthritis and Sjogren’s syndrome.

Having a moderate/having a high/having a slight fever

Frequent/occasional unexplained fevers

Numb/tingling/burning extremities
Rheumatoid arthritis can cause peripheral neuropathy leading to paresthesia.

(Prolonged) morning stiffness

Joint pain/swelling/stiffness

Heberden's nodes

Red palms/fingertips

Lighter/paler skin color
Conditions that suggest Rheumatoid Arthritis



Low DHEA Level
DHEA levels have been found to be low in women with rheumatoid arthritis, a condition frequently associated with osteoporosis. In a study of 49 postmenopausal women with rheumatoid arthritis, DHEA levels (measured as DHEA-S ) were significantly lower than in healthy controls. [Gaby, AR. Holistic Medicine. Spring, 1993: p.22]


Weakened Immune System
People with rheumatoid arthritis, who for a long time were thought to have overactive immune systems, instead may have exhausted immune systems. A study at the Mayo Clinic has shown for the first time that patients with rheumatoid arthritis have prematurely aged immune systems. Patients 20 to 30 years old had a collection of T-cells that looked like they belonged to 50 to 60 year olds.

Immune System Imbalance (TH2 Dominance)
A Mayo Clinic study found that the T-cells were ‘worn out’ in rheumatoid arthritis patients, who do not make new T-cells as readily as they should.



Osteoporosis / Risk
According to researchers, women with rheumatoid arthritis have up to double the risk of developing osteoporosis and those who use steroid drugs to help control the arthritis are at an even higher risk of bone loss. [Arthritis and Rheumatism, March 2000]


Zinc Requirement
There is a possibility that zinc malabsorption may contribute to low zinc levels amongst rheumatoid arthritics. [J Rheumatol. 1997;24(4): pp.643-646] While levels of zinc have been found to be lower than normal in the blood of patients with rheumatoid arthritis, supplementation does not appear to be beneficial to the condition.

Dry Eye
“Dry eye” is a symptom of certain autoimmune diseases like rheumatoid arthritis and Sjogren’s syndrome.

Night Sweats
Night sweats, depression and lethargy can accompany this disease.
Rheumatoid arthritis
Counter Indicators
Absence of rheumatoid arthritis
Risk factors for Rheumatoid Arthritis

Ulcerative Colitis
Joint inflammation can occur from the overactive immune system seen in ulcerative colitis. This problem may go away when the colitis is treated.

Pericarditis
Sometimes pericarditis may be a secondary symptom of rheumatoid arthritis.


Atrophic Gastritis
Chronic atrophic gastritis occurs in up to 63% of rheumatoid arthritis patients. Achlorhydria also occurs frequently and is associated with changes in gastric microbial patterns.



Dysbiosis, Bacterial
Immunologic responses to gut flora have been advanced by several authors as being important causative factors of inflammatory joint diseases. It is well-known that reactive arthritis can be activated by intestinal infections with Yersinia, Salmonella and other enterobacteria. In some cases bacterial antigens have been found in synovial cells and may enter the circulation because of the increased intestinal permeability associated with the intestinal infection. Increased intestinal permeability and immune responses to bacterial debris may cause other types of inflammatory joint disease as well.

(Highly) elevated CRP level
Increased blood levels of C-reactive protein (CRP) are seen long before symptoms of rheumatoid arthritis appear.

EFA (Essential Fatty Acid) Type 3 Requirement
Aching, swollen joints may just be demanding the right kind of oil. Shifting the body’s balance toward omega-3 oils and away from omega-6 oils significantly alleviates symptoms in patients with rheumatoid arthritis, according to a recent study in the Journal of Rheumatology.




History of rheumatoid arthritis
Rheumatoid Arthritis suggests the following may be present

Autoimmune Tendency
It is quite clear that autoimmunity plays a major role in the progression of rheumatoid arthritis.

Chronic Thyroiditis
A study of 91 patients with rheumatoid arthritis found 29 patients had evidence of thyroid dysfunction compared to 10 of the
93 controls. The excess thyroid dysfunction was due to either hypothyroidism or Hashimoto’s thyroiditis. In this study, thyroid dysfunction is seen at least 3 times more often in women with rheumatoid arthritis than in women with similar demographic features with non-inflammatory rheumatoid diseases such as osteoarthritis and fibromyalgia. [Annals of Rheumatic Diseases, 1993;52 pp.454-456]


Atrophic Gastritis
Chronic atrophic gastritis occurs in up to 63% of rheumatoid arthritis patients. Achlorhydria also occurs frequently and is associated with changes in gastric microbial patterns.

Hydrochloric Acid Deficiency
Lack of stomach acid occurs frequently in rheumatoid arthritis patients. This is associated with changes in gastric microbial patterns.

Low DHEA Level
DHEA levels have been found to be low in women with rheumatoid arthritis, a condition frequently associated with osteoporosis. In a study of 49 postmenopausal women with rheumatoid arthritis, DHEA levels (measured as DHEA-S ) were significantly lower than in healthy controls. [Gaby, AR. Holistic Medicine. Spring, 1993: p.22]

Hypothyroidism
A study of rheumatoid arthritis patients found evidence of thyroid dysfunction 3 times more often than in controls. The excess thyroid dysfunction was due to either hypothyroidism or Hashimoto’s thyroiditis. [Annals of Rheumatic Diseases, 1993;52 pp.454-456]
Weakened Immune System
People with rheumatoid arthritis, who for a long time were thought to have overactive immune systems, instead may have exhausted immune systems. A study at the Mayo Clinic has shown for the first time that patients with rheumatoid arthritis have prematurely aged immune systems. Patients 20 to 30 years old had a collection of T-cells that looked like they belonged to 50 to 60 year olds.

Dysbiosis, Bacterial
Immunologic responses to gut flora have been advanced by several authors as being important causative factors of inflammatory joint diseases. It is well-known that reactive arthritis can be activated by intestinal infections with Yersinia, Salmonella and other enterobacteria. In some cases bacterial antigens have been found in synovial cells and may enter the circulation because of the increased intestinal permeability associated with the intestinal infection. Increased intestinal permeability and immune responses to bacterial debris may cause other types of inflammatory joint disease as well.


Osteoporosis / Risk
According to researchers, women with rheumatoid arthritis have up to double the risk of developing osteoporosis and those who use steroid drugs to help control the arthritis are at an even higher risk of bone loss. [Arthritis and Rheumatism, March 2000]
Rheumatoid Arthritis can lead to


Rheumatoid Arthritis could instead be

Lyme Disease
The symptoms of Lyme disease have frequently been misdiagnosed as rheumatoid arthritis and subsequently mistreated.
Recommendations for Rheumatoid Arthritis

Phenylalanine
The ‘D’ form of phenylalanine (DPA) has been used to treat chronic pain, including rheumatoid arthritis, with mixed effectiveness.
Thymic Factors
The thymus gland contributes to the maturing of T-cells. Thymus gland extracts will assist this process when the thymus gland is shrunken, as happens commonly in aging. Through his clinical experiences with thymic supplementation, Dr. Burgstiner said he observed 28 cases of rheumatoid arthritis cases go into remission where patients no longer needed to use prednisone, methotrexate, or gold shots.
Cetyl-myristoleate
In a small study of patients with severe to crippling rheumatoid arthritis, 4 were unable to walk, and one could not sit in a wheelchair. After 20 days, 5 showed improvement, and 3 were totally free of pain with almost complete return of joint mobility. All but two were totally pain-free and had recovered mobility in their joints. One of the two had abused steroids as an athlete and the other had cirrhosis of the liver.
In those with mild to moderately severe rheumatoid arthritis, after 14 days of treatment, 9 patients reported continuing improvement even though treatment had completed. (Unpublished study)

Fish Oil / Krill
Beside the comments under essential fatty acids, please see the link between Rheumatoid Arthritis and Vegetarian Diet.

Turmeric Extract, Curcumin
Clinical studies have substantiated curcumin anti-inflammatory effects, including a significant beneficial effect in Rheumatoid Arthritis. In one study, curcumin was compared to phenylbutazone, a very potent NSAID that has fallen out of favor because of frequent side effects. The improvements in the duration of morning stiffness, walking time, and joint swelling were comparable in both groups.

Cat's Claw (Urticaria tomentosa)
Uncaria tomentosa extract over a 6 month period reduced the number of painful joints in a well-controlled study involving 40 patients with active rheumatoid arthritis already being treated with sulfasalazine or hydroxychloroquine. An additional 7 months of treatment with Uncaria tomentosa extract reduced the number of painful and swollen joints with the same group of patients. [J Rheumatol 2002;29(4): pp.678-81]

Evening Primrose Oil / GLA
Scientists at the University of Pennsylvania reported that high doses of GLA helps in treating rheumatoid arthritis patients. An earlier study by them had shown that administration of 1100mg of GLA per day from borage seed oil reduced synovitis in six of seven patients with rheumatoid arthritis.
The anti-inflammatory properties of EPO have been studied in double-blind research with people suffering from rheumatoid arthritis. Some, but not all, studies have reported that EPO supplementation provides significant benefit to these people.

Antiinflammatory Combination Products
Some combination products contain enzymes which have anti-inflammatory activity as well as other ingredients which may have fibrinolytic, immune modulating and blood cleansing effects too.

Cayenne Pepper (Capsicum frutescens)
Topically for pain control only.


Picrorhiza (Picrorhiza kurroa)
Open-label studies conducted in India show a preliminary benefit for persons with primarily rheumatoid arthritis. [Langer JG, Gupta OP, Atal CK (1981) “Clinical trials on Picrorhiza kurroa” Ind J Pharmacol 13: pp.98-103 (review)] More study is needed before any definite conclusions can be drawn.
See also [T Hart BA, Simons JM, Knaan-Shanzer S, et al. Antiarthritic activity of the newly developed neutrophil oxidative burst antagonist apocynin. Free Rad Biol Med 1990;9: pp.127-31]


Lei Gong Teng (Tripterygium wilfordii Hook F)
Treatment with an extract of Tripterygium wilfordii Hook F (360mg per day to 570mg per day) improved clinical anifestations and laboratory findings in a study of 13 patients with rheumatoid arthritis. Three patients withdrew during the first 16 weeks of
dose escalation, including one patient who developed diastolic hypertension at a dose of 180mg per day. [J Rheumatol 2001;28(10): pp.2160-7]

Liver/Gall Bladder Flush
It is commonly reported that arthritic symptoms decrease with repeated liver/gallbladder flushes.
Vegetarian/Vegan Diet
Researchers in one study found that participants who ate the greatest number of servings of cooked vegetables were about 75% less likely to develop rheumatoid arthritis than those who reported eating the fewest servings. [American Journal of Clinical Nutrition: November 1999;70: pp.1077-1082]
“… 43 patients with rheumatoid arthritis, those assigned to a vegan diet… had improvement in rheumatoid arthritis symptoms.” [British J Rheumatology, 36(1) 1997]
Another study found that of 22 patients with rheumatoid arthritis who completed 9 months of a vegan diet that did not contain any dairy products or gluten, 40% noted an improvement in symptoms compared with minimal improvement in rheumatoid arthritic patients who consumed a non vegan diet. [Rheumatolozy 2001;40: pp.1175-1179]
Rheumatoid arthritis patients consumed either the typical Western diet or an antiinflammatory diet, which was a modified lactovegetarian diet for an 8-month period. Patients in both groups received either placebo or an oil which provided 30mg of total fish oil omega-3 fatty acids (EPA, DHA) per kg of body weight. Those on the antiinflammatory diet compared with the Western diet experienced a reduction in tender and swollen joints by 14% during the placebo treatment while during the fish oil supplementation, the antiinflammatory diet compared with the Western diet had a reduction in the number of tender joints at 28% versus 11%, respectively, and swollen joints at 34% versus 22%, respectively. [Rheumatol Int. 2003;23:27-36]
Increased Fruit/Vegetable Consumption
Please see the link between RA and Vegetarian Diet.

Monounsaturated Oils
Researchers found that people who used the most olive oil were significantly less likely to develop rheumatoid arthritis than people who consumed the least. [American Journal of Clinical Nutrition: November 1999;70: pp.1077-1082]

Dairy Products Avoidance
Here is a letter received by Robert Cohen, arch enemy of the dairy industry and despised by most dairy farmers. The letter was sent to him in January, 2002 by a long-time dairy farmer and speaks for itself:
You and I have stood on different sides of the fence for a number of years, but I’ve got a story to tell you, and an apology to offer. Catherine (my wife of 21 years) and I both grew up on dairy farms. We’ve been raising Holsteins as long as we can remember. Cath is just 42 years old, but she is crippled with rheumatoid arthritis. There is no record of this disease in her family, but she has been in pain for the past two years, much of it bedridden.
We’ve tried traditional and alternative therapies and medicines, but she only got a little short term relief. We even tried acupuncture. Try finding an acupuncturist in the rural Midwest! It was expensive, and didn’t really work. Catherine’s pain has been unbearable at times.
Despite there being no information on the internet linking dairy consumption to rheumatoid arthritis, and nothing in medical journals (I’ve searched online Medline), we made a resolution together to discontinue drinking our own milk, and not eat cheese or any other dairy product for six months, just to see if there would be some improvement.
I have to tell you this. Catherine feels like she’s been to Lourdes. She’s cured. There is some pain, but most is gone. I’ve had changes too which I’ll discuss some other time. I thank you, and curse you at the same time. Milking cows is my livelihood. I’ve always believed that what I was doing was the right thing. I’m not going to sell my cows and sell my farm. I love the business. I just don’t feel that good about it anymore. You were right about the arthritis. I don’t know about the cancer and heart attacks, but you have given us a miracle that doctors were not able to provide. It did not take us three to six months to learn the truth. It took just three weeks. I’ve ridiculed your work in the past. Please accept my apology.
Your friend,
Tom
Since this type of joint pain can be a symptom of food allergy, dietary change may have a profound effect. Dairy products – the most common food allergen, are one likely causative factor.
“In the case of the eight year old female subject, juvenile rheumatoid arthritis was a milk allergy. After avoiding dairy products, all pain was gone in three weeks.” [Journal of the Royal Society of Medicine, 1985, 78]
“In systemic arthritis, like Rheumatoid, the cause is coursing through the blood, and it got there through the diet. When all of the joints are involved, the cause is not physical, but chemical. It’s usually casein. (Eighty percent of milk protein is casein).” [“No Milk”, by Daniel Twogood, D.C.]
“Certain foods trigger the symptoms of rheumatoid arthritis, and eliminating these foods sometimes causes even long-standing symptoms to improve or even remit entirely. It is important to avoid the problem foods completely, as even a small amount can cause symptoms. All dairy products should be avoided: skim or whole cow’s milk, goat’s milk, cheese, yogurt, cream, etc.” [Neal Barnard, M.D. Physicians Committee for Responsible Medicine]

Therapeutic Fasting
The fast allows the entire system to restore its cellular and immunogenic integrity. Fasting can cause regression of some autoimmune and inflammatory disorders, such as rheumatoid arthritis. [Controlled trial of fasting and a one-year vegetarian diet eased symptoms of rheumatoid arthritis. The Lancet, 1991, 338]

Nightshade Food Avoidance
Elimination of nightshade family foods does not help all people with arthritis, but people who respond are usually helped a great deal.
According to a study conducted in 1993 by Childers, eating nightshade foods results in “a buildup of cholinesterase inhibiting glycoalkaloids and steroids …and may cause inflammation, muscle spasms, pain, and stiffness.” The less cholinesterase the body produces as it ages, the less agile the body will be. Therefore, anything that additionally inhibits cholinersterase will add to joint deterioration and stiffness. Cholinesterase inhibitors such as nightshade foods affect mostly rheumatoid-type arthritis.

LDN - Low Dose Naltrexone
Ten patients with this disease have been treated with LDN in recent years. In all ten patients the joint pain and swelling cleared, in some, leaving residual joint distortion. Two of the patients stopped LDN for several weeks because of travel. Both had an immediate exacerbation. One patient who was responding well on LDN had a mild exacerbation during a period of severe marital stress.

Conventional Drugs / Information
Sulfasalazine is a prodrug, that is, it is not active in its ingested form. It is broken down by bacteria in the colon into two products: 5-aminosalicylic acid (5ASA), and sulfapyridine. There is some controversy as to which of these two products are responsible for the activity of azulfidine. Whereas it is known that 5ASA has therapeutic benefit, it is not clear whether sulfapyridine adds any further benefit. In the colon, the products created by the breakdown of sulfasalazine work as anti-inflammatory agents for treating inflammation of the colon. The beneficial effect of sulfasalazine is believed to be due to a local effect on the bowel, although there may also be a beneficial systemic immune-suppressant effect as well. Following oral administration, 33% of the sulfasalazine is absorbed, all of the sulfapyridine is absorbed, and about 33% of the 5ASA is absorbed. Sulfasalazine was approved by the FDA in 1950.
Plaquenil may be used for short or long-term rheumatoid arthritis treatment. In treating rheumatoid arthritis, Plaquenil may slow down the substances which harm the joints.
Centocor, Inc., Schering-Plough Corporation, and Mitsubishi Tanabe Pharma Corporation have announced that an estimated one million patients have now been treated with REMICADE® (infliximab), the leading anti-tumor necrosis factor (TNF)-alpha therapy worldwide (2007). In fact, REMICADE has been used to treat more patients worldwide than all other anti-TNF-alpha agents combined. REMICADE was the first anti-TNF-alpha treatment approved by the U.S. Food and Drug Administration (FDA), when it was indicated for the treatment of acute moderate to severe Crohn’s disease in 1998. The indication for Crohn’s disease was quickly followed by additional indications, such as rheumatoid arthritis.
“Rheumatoid arthritis derailed my life,” said Ellen Shmueli, RA patient. “Simple tasks like lifting my child or holding a pen were nearly impossible. It’s hard to put into words what REMICADE has meant to me.”
Through a long line of firsts in the biotechnology industry, the history of REMICADE includes 15 FDA indications spanning across inflammatory diseases that include Crohn’s disease (adult and pediatric), ulcerative colitis, rheumatoid arthritis (RA), ankylosing spondylitis, psoriatic arthritis and psoriasis.
“This significant milestone was achieved as a result of nearly three decades of expanding and improving access for people living with life-altering inflammatory diseases,” said Neal Fowler, President, Centocor, Inc. “In partnership with Centocor R&D, we will continue our pledge of bringing the promise of biomedicine to physicians and patients through continued research and development, REMICADE and our promising pipeline portfolio.”
REMICADE has been studied in more than 37 clinical trials, evaluating its use in a wide variety of diseases of the immune system and is approved for use in 88 countries.

Antibiotics
Antibiotic therapy has been controversial. Doctors haven’t proved, or disproved, that an infection causes rheumatoid arthritis. Early studies of minocycline showed only a modest effect, discouraging many physicians, said Dr. Doyt Conn of The Arthritis Foundation.
Most rheumatology investigators believe that an infectious agent causes rheumatoid arthritis. There is little agreement as to the involved organism. Investigators have proposed the following infectious agents: Human T-cell lymphotropic virus Type I, rubella virus, cytomegalovirus, herpesvirus, and mycoplasma. There is evidence supporting the hypothesis that mycoplasma is a common etiologic agent of rheumatoid arthritis.
Minocycline is a more potent antibiotic than tetracycline and penetrates tissues better. These characteristics shifted the treatment of rheumatic illness away from tetracycline to minocycline. Minocycline may benefit rheumatoid arthritis patients through its immunomodulating and immunosuppressive properties as well.
Thinking that treatment earlier in the disease might work better, 46 patients were treated who had rheumatoid arthritis for less than a year and were not taking strong arthritis medicines. Sixty-five percent of the minocycline patients showed a 50% improvement in joint swelling, stiffness and pain after six months of therapy. Just 13% of patients given a dummy pill had a similar response. How long improvement lasted was key, because many other treatments either wear off or eventually cause serious side effects. Over a period of three years, 44% ultimately improved by a dramatic 75% or more.
Such improvement over time is encouraging, said Dr. Eric Schned, a Minneapolis rheumatologist who has followed O’Dell’s work.
The definitive scientific support for minocycline in the treatment of rheumatoid arthritis came with the MIRA trial in the United States. This was a double blind randomized placebo controlled trial done at six university centers involving 200 patients for nearly one year. The dosage they used (100mg BID) was much higher and likely more effective than what most clinicians were using. They also did not employ any additional antibiotics or nutritional regimens, yet 55% of the patients improved. This study finally provided the “proof” that many traditional clinicians demanded before seriously considering this treatment as an alternative regimen for rheumatoid arthritis.
Chemical Avoidance
Frequent Oil Changes Linked to Rheumatoid Arthritis.
Changing the oil frequently may not help the joints. Occupational exposure to mineral oils, particularly hydraulic and motor oils, increases the risk of developing rheumatoid arthritis by 60% in certain groups of patients, researchers here say.
Exposure increased the risk for rheumatoid factor-positive arthritis but not RF-negative arthritis, said Lars Klareskog, Ph.D., of the Karolinska Institute here and colleagues reported in a study published online by Arthritis Research & Therapy. [Sverdrup B et al. Association between occupational exposure to mineral oil and rheumatoid arthritis: results from the Swedish EIRA case-control study. Arthritis Research & Therapy. 2005; 7:R1296-R1303.]

Plant Sterols / Sterolins (Phytosterols)
In a clinical model of chronic inflammation, rheumatoid arthritis patients were followed over a period of 6 months and this study (double-blind, placebo-controlled) showed attenuation of indices of disease activity due to the potent anti-inflammatory properties of the sterols/sterolins. [Am. J. Clin. Nutr. J (2002) 75, Abstract 40, 351S]

Fibrinolytic Enzymes
Some fibrinolytic enzyme products contain other enzymes as well, giving them anti-inflammatory, fibrinolytic, immune modulating and blood cleansing effects. Vitalzym is one such product.

DHEA
The incidence of osteoporosis is elevated in women with rheumatoid arthritis. DHEA levels correlated significantly with, and were predictive of, bone mineral density, even after corticosteroid therapy was taken into account. Raising DHEA levels by supplementation in these women should reduce the risk of osteoporosis. [Gaby, AR. Holistic Medicine. Spring, 1993: p.22]
Dr. Hackethal has observed some rheumatoid patients taking DHEA become well even when C-reactive protein and Rh- factor are positive.

Progesterone
Topical progesterone has been reported to be useful in alleviating symptoms.

Test for Food Allergies
While virtually any food can result in aggravation of rheumatoid arthritis, the most common offending foods are dairy protein, wheat, corn, citrus fruits, eggs, beef, sugar, fats, salt, caffeine and nightshade (Solanum) family foods (tomato, potato, eggplants, peppers and tobacco).
In order to test whether foods trigger symptoms, a food elimination protocol was followed in a blind, placebo-controlled study that resulted in significant improvement in arthritic symptoms, including shorter duration of morning stiffness and fewer painful joints. [Lancet 1986:1, pp.236-8]
While many doctors believe that the percentage of rheumatoid arthritis patients benefiting from diet manipulation is small, there is an increasing number of scientific studies suggesting that food elimination may help a higher percentage of patients.
“Nutritional therapy, not drugs, is the cornerstone of alternative treatment. A treatment for arthritis that relieves symptoms in a large percentage of patients is based on the theory that most arthritic symptoms are allergic reactions.” [Jane Heimlich (wife of Dr. Henry Heimlich, the “Heimlich Maneuver” physican), in her book, “What Your Doctor Won’t Tell You”]

Test Zinc Levels
Zinc levels amongst patients with rheumatoid arthritis are usually reduced. Results from zinc supplementation trials amongst rheumatoid arthritis patients have been mixed, though most find some improvement.


Manganese
Manganese functions in the antioxidant enzyme superoxide dismutase (manganese SOD), which is deficient in patients with rheumatoid arthritis. Manganese supplementation has been shown to increase SOD activity, indicating increased antioxidant activity. A good dosage for a manganese supplementation is 5 to 15mg per day.

Selenium
Selenium levels are generally low in patients with rheumatoid arthritis. Low selenium levels in joint tissues may be a significant factor contributing to the inflammatory process in rheumatoid arthritis. Selenium plays an important role as an antioxidant and serves as the mineral cofactor in the free-radical scavenging enzyme glutathione peroxidase. This enzyme is also important in reducing the production of inflammatory compounds that cause much of the damage to tissues seen in rheumatoid arthritis. A deficiency of selenium would result in even more significant damage.

Boron
There is increasing evidence that boron is an essential trace element for both man and animal. It does influence calcium and magnesium metabolism, and this is possibly through the parathyroid gland. It does alleviate and seems to cure arthritis either by acting against whatever organism may cause rheumatoid diseases and/or as a membrane catalyst that permits repair of damaged cartilage and collagen.

Copper
Copper has a mild anti-inflammatory effect. The use of copper bracelets in the treatment of arthritis has a long history, and wearers continue to claim positive results. The copper in the bracelets reacts with the fatty acids in the skin to form copper salts that are absorbed into the body. The copper salts may cause a blue-green stain on the skin, but this can be removed with soap and water. Recent research suggests that copper salicylate used to treat arthritis reduces symptoms more effectively than either copper or aspirin alone.

MSM (Methyl Sulfonyl Methane)
The reason why MSM is beneficial against arthritis is unclear. It may be because of its sulfur content, or because of its anti-inflammatory and analgesic properties. Unlike aspirin, which offers immediate pain relief, MSM takes 3 to 4 weeks before it produces noticeable change, except in rheumatoid patients who have been known to feel differences in just one day, and almost always within 3 to 4 days.
In an animal study on rheumatoid arthritis-like joint degeneration, MSM was effective in reducing joint inflammation, and completely prevented the breakdown of cartilage. According to Dr. Stanley Jacobs, MD, MSM can be helpful in most musculoskeletal pain and inflammation, including rheumatoid arthritis.


Essential Fatty Acids
Both Omega 6 and Omega 3 EFAs and their metabolites Gamma Linolenic Acid (GLA) and EPA have shown effectiveness in Rheumatoid Arthritis. One study showed that use for 12 months produced meaningful improvement in 76% of subjects. The oil from cold water fish falls into the Omega 3 category, and has shown positive results in reducing inflammation. Some researchers believe that if you regularly eat small amounts of cold-water fish (which contain Omega 3 fatty acids) over many years, you may be able to avoid rheumatoid arthritis.
In a review that was completed by the medical research firm, Metaworks, Inc. in Medford Mass, lead researcher Dr. Marya Zilberberg reported that GLA is not only safe, but it is also an effective natural therapy. In her review of close to 40 clinical papers on GLA, she noted that GLA consistently reduces inflammation and joint stiffness without any of the serious side effects associated with pharmaceutical drugs. Zilberberg found that GLA is particularly useful for reducing morning stiffness. “We saw about a 60-65% reduction in morning stiffness for these patients,” said Zilberberg. “In other words if you have two hours of morning stiffness, that goes down to about a half hour. It is an extremely striking difference.”
Also see the link between Rheumatoid Arthritis and Vegetarian Diet.

Superoxide Dismutase
In a Danish study, arthritis patients were treated with injections of superoxide dismutase, an enzyme containing copper (or manganese and zinc) that is found within the cells. Many obtained relief from symptoms such as joint swelling, pain and morning stiffness.
Ozone / Oxidative Therapy
Many people with arthritis report that the hydrogen peroxide bath has helped them greatly.
International studies are finding that hyperbaric oxygen therapy is markedly superior to the routine treatment of RA. In 1995, the Proceedings of the Eleventh International Congress on Hyperbaric Medicine published the results of one particular study. These results indicated the following effects of hyperbaric oxygen on the disease.
Remission: 23.4%
Obvious effect: 51.4%
Improvement: 16.2%
No effect: 8.1%
The total summarized effective rate of hyperbaric oxygen in treating RA was 91.9%. The authors of the study concluded, “In the treatment we find that hyperbaric oxygen is markedly superior to the routine treatment of rheumatoid arthritis.” From PatientsMedical.com.

Calming / Stretching Exercises
According to a 1994 study published in the British Journal of Rheumatology, 20 patients with rheumatoid arthritis participated in a yoga program. Left hand grip strength improved significantly and all patients who completed the course expressed the desire to continue after the study.

Leeches
Applying leeches to involved joints in rheumatoid patients reduced muscle and joint pain, duration of early morning stiffness, improved joint range of motion and functional activity, and reduced erythrocyte sedimentation rate, C reactive protein, prothrombin index (PTI), activated partial thromboplastin time (APTT) and prolonged coagulation time without any adverse effects being reported. [2002 European Congress of Rheumatology, June12-15, 2002, Stockholm, Sweden]
Vitamin D
A small clinical trial for RA and a vitamin D metabolite was conducted over a three-month time period. The results were positive: “Therapy showed a positive effect on disease activity in 89% of the patients (45% with complete remission and 45% with a satisfactory effect). Only two patients (11%) showed no improvement, but no new symptoms occurred”. [Clin. Exp. Rheumatol. 1999 (17): pp. 453-456] Also see the link between Autoimmune Tendency and Vitamin D.
Researchers have found women who eat a diet rich in vitamin D may reduce their chances of developing rheumatoid arthritis (RA) and multiple sclerosis (MS). Two studies involving women have shown proof of the vitamin’s benefits.
The RA study followed 29,368 women aged 55 to 69 years, and the MS study looked at more than 185,000 women. The participants were given questionnaires to fill out about their dietary habits and vitamin D intake at the beginning of each study, and researchers followed up with the women every four years for up to 20 years. They discovered that women were 30 percent less likely to develop RA, and 40 percent less likely to develop MS, when taking the recommended daily amount or more of vitamin D.
Out of 100 people worldwide, one or two will develop RA and around 0.04 percent have MS. Both of these conditions are thought to occur when the body’s immune system turns against itself. Researchers suggest that vitamin D may work by calming overactive immune cells.
Responding to this study, vitamin D experts advise future researchers studying vitamin D levels to administer a blood test to read the levels more accurately, and cautioned that this study did not use the best way to determine vitamin D levels in the participants. [Neurology January, 2004 13;62(1):60-5, Arthritis & Rheumatism January, 2004;50(1):72-7]
Dr. Joseph Mercola, D.O. reports that he has “seen several hundred patients with rheumatoid arthritis in the last two years, and I have measured their levels. I have yet to analyze the results, but I cannot recall any RA patients who had normal levels of vitamin D. In fact, it is so consistent that I immediately start any new patient who comes in with RA on supplemental vitamin D, in addition to vitamin D in cod liver oil.”

Vitamin B6 (Pyridoxine)
When nodules (Heberden’s nodes) are present, vitamin B6 at 100-150mg per day may help. One doctor reports seeing even better results if one handful of raw pecans is eaten every day. The nodes may not go away but pain and mobility are better over several weeks.

Vitamin B5 (Pantothenic Acid)
Low pantothenic acid levels are implicated in the development of human osteoarthritis and rheumatoid arthritis, as whole blood pantothenic acid levels have been reported to be lower in rheumatoid arthritis patients compared with normal controls. In addition, disease activity was inversely correlated with pantothenic acid levels.
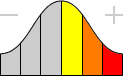
Key
 | Weak or unproven link |
 | Strong or generally accepted link |
 | Proven definite or direct link |
 | Weakly counter-indicative |
 | Very strongly or absolutely counter-indicative |
 | May do some good |
 | Likely to help |
 | Highly recommended |
Glossary
Rheumatoid Arthritis
A long-term, destructive connective tissue disease that results from the body rejecting its own tissue cells (autoimmune reaction).
Arthritis
Inflammation of a joint, usually accompanied by pain, swelling, and stiffness, and resulting from infection, trauma, degenerative changes, metabolic disturbances, or other causes. It occurs in various forms, such as bacterial arthritis, osteoarthritis, or rheumatoid arthritis. Osteoarthritis, the most common form, is characterized by a gradual loss of cartilage and often an overgrowth of bone at the joints.
Malaise
A vague feeling of bodily discomfort, as at the beginning of an illness. A general sense of depression or unease.
Bacteria
Microscopic germs. Some bacteria are "harmful" and can cause disease, while other "friendly" bacteria protect the body from harmful invading organisms.
Antigen
A substance, usually protein or protein-sugar complex in nature, which, being foreign to the bloodstream or tissues of an animal, stimulates the formation of specific blood serum antibodies and white blood cell activity. Re-exposure to similar antigen will reactivate the white blood cells and antibody programmed against this specific antigen.
Immune System
A complex that protects the body from disease organisms and other foreign bodies. The system includes the humoral immune response and the cell-mediated response. The immune system also protects the body from invasion by making local barriers and inflammation.
Antibody
A type of serum protein (globulin) synthesized by white blood cells of the lymphoid type in response to an antigenic (foreign substance) stimulus. Antibodies are complex substances formed to neutralize or destroy these antigens in the blood. Antibody activity normally fights infection but can be damaging in allergies and a group of diseases that are called autoimmune diseases.
Protein
Compounds composed of hydrogen, oxygen, and nitrogen present in the body and in foods that form complex combinations of amino acids. Protein is essential for life and is used for growth and repair. Foods that supply the body with protein include animal products, grains, legumes, and vegetables. Proteins from animal sources contain the essential amino acids. Proteins are changed to amino acids in the body.
pH
A measure of an environment's acidity or alkalinity. The more acidic the solution, the lower the pH. For example, a pH of 1 is very acidic; a pH of 7 is neutral; a pH of 14 is very alkaline.
T-Cell
T cells are lymphocytes that are produced in the bone marrow and mature in the thymus. T cells are responsible for mediating the second branch of the immune system called "cellular immune response." T cells can live for months to years. This lymphocyte population is defined by the presence of a rearranged T-cell receptor.
Virus
Any of a vast group of minute structures composed of a protein coat and a core of DNA and/or RNA that reproduces in the cells of the infected host. Capable of infecting all animals and plants, causing devastating disease in immunocompromised individuals. Viruses are not affected by antibiotics, and are completely dependent upon the cells of the infected host for the ability to reproduce.
Cartilage
Specialized fibrous connective tissue that forms the skeleton of an embryo and much of the skeleton in an infant. As the child grows, the cartilage becomes bone. In adults, cartilage is present in and around joints and makes up the primary skeletal structure in some parts of the body, such as the ears and the tip of the nose.
White Blood Cell
(WBC): A blood cell that does not contain hemoglobin: a blood corpuscle responsible for maintaining the body's immune surveillance system against invasion by foreign substances such as viruses or bacteria. White cells become specifically programmed against foreign invaders and work to inactivate and rid the body of a foreign substance. Also known as a leukocyte.
Rheumatism
General term applied to conditions of pain, or inability to articulate, various elements of the musculoskeletal system.
Anemia
A condition resulting from an unusually low number of red blood cells or too little hemoglobin in the red blood cells. The most common type is iron-deficiency anemia in which the red blood cells are reduced in size and number, and hemoglobin levels are low. Clinical symptoms include shortness of breath, lethargy and heart palpitations.
Red Blood Cell
Any of the hemoglobin-containing cells that carry oxygen to the tissues and are responsible for the red color of blood.
Autoimmune Disease
One of a large group of diseases in which the immune system turns against the body's own cells, tissues and organs, leading to chronic and often deadly conditions. Examples include multiple sclerosis, rheumatoid arthritis, systemic lupus, Bright's disease and diabetes.
Neuropathy
A group of symptoms caused by abnormalities in motor or sensory nerves. Symptoms include tingling or numbness in hands or feet followed by gradual, progressive muscular weakness.
Paresthesia
A skin sensation, such as burning, prickling, itching, or tingling, with no apparent physical cause.
DHEA
Dehydroepiandrosterone (DHEA) is a steroid produced by the adrenal glands and is the most abundant one found in humans. DHEA may be transformed into testosterone, estrogen or other steroids. It is found in the body as DHEA or in the sulfated form known as DHEA-S. One form is converted into the other as needed.
Osteoporosis
A disease in which bone tissue becomes porous and brittle. The disease primarily affects postmenopausal women.
Steroid
Any of a large number of hormonal substances with a similar basic chemical structure containing a 17-carbon 14-ring system and including the sterols and various hormones and glycosides.
Zinc
An essential trace mineral. The functions of zinc are enzymatic. There are over 70 metalloenzymes known to require zinc for their functions. The main biochemicals in which zinc has been found to be necessary include: enzymes and enzymatic function, protein synthesis and carbohydrate metabolism. Zinc is a constituent of insulin and male reproductive fluid. Zinc is necessary for the proper metabolism of alcohol, to get rid of the lactic acid that builds up in working muscles and to transfer it to the lungs. Zinc is involved in the health of the immune system, assists vitamin A utilization and is involved in the formation of bone and teeth.
Ulcerative Colitis
(Colitis ulcerosa): Ulceration of the colon and rectum, usually long-term and characterized by rectal bleeding or blood in the stool, frequent urgent diarrhea/bowel movements each day, abdominal pain.
Colitis
Inflammation of the colon.
Chronic
Usually Chronic illness: Illness extending over a long period of time.
Atrophic Gastritis
Chronic inflammation of the stomach that causes the breakdown of the mucous membranes and a reduction in the number of functioning stomach cells. Seen mainly in the elderly.
Achlorhydria
The complete absence or failure of stomach acid secretion.
CRP
C-reactive protein. A sensitive measure of inflammation in the body.
Thyroid
Thyroid Gland: An organ with many veins. It is at the front of the neck. It is essential to normal body growth in infancy and childhood. It releases thyroid hormones - iodine-containing compounds that increase the rate of metabolism, affect body temperature, regulate protein, fat, and carbohydrate catabolism in all cells. They keep up growth hormone release, skeletal maturation, and heart rate, force, and output. They promote central nervous system growth, stimulate the making of many enzymes, and are necessary for muscle tone and vigor.
Hypothyroidism
Diminished production of thyroid hormone, leading to low metabolic rate, tendency to gain weight, and sleepiness.
Fibromyalgia
(FMS): Originally named fibrositis, it is a mysteriously debilitating syndrome that attacks women more often than men. It is not physically damaging to the body in any way, but is characterized by the constant presence of widespread pain that often moves about the body. Fibromyalgia can be so severe that it is often incapacitating.
Stomach
A hollow, muscular, J-shaped pouch located in the upper part of the abdomen to the left of the midline. The upper end (fundus) is large and dome-shaped; the area just below the fundus is called the body of the stomach. The fundus and the body are often referred to as the cardiac portion of the stomach. The lower (pyloric) portion curves downward and to the right and includes the antrum and the pylorus. The function of the stomach is to begin digestion by physically breaking down food received from the esophagus. The tissues of the stomach wall are composed of three types of muscle fibers: circular, longitudinal and oblique. These fibers create structural elasticity and contractibility, both of which are needed for digestion. The stomach mucosa contains cells which secrete hydrochloric acid and this in turn activates the other gastric enzymes pepsin and rennin. To protect itself from being destroyed by its own enzymes, the stomach’s mucous lining must constantly regenerate itself.